Abstract
Chymotrypsin-like serine proteases are hallmarked by a protease domain comprising the catalytic triad residues His57, Asp102, and Ser195 (chymotrypsinogen numbering) situated in the active site cleft. While the catalytic triad in conjunction with the oxyanion hole residues regulate substrate cleavage, the active site subpockets (S1-4) control substrate recognition and binding. The high structural homology of the serine protease domains allows for analogous strategies in drug design, which is underscored by the direct oral anticoagulants (DOACs) for the prophylactic management of stroke in atrial fibrillation and prevention and treatment of venous thrombosis. DOACs inhibit coagulation serine proteases by reversibly engaging the active site with high affinity. To expand the repertoire of DOAC-specific reversal agents we have previously successfully modified the S4 active site subpocket of human factor Xa to prevent DOAC binding while preserving catalytic activity [Verhoef 2017 Nature Commun.]. To explore whether an analogous strategy can be applied to create DOAC resistance in the serine protease thrombin, specific substitutions or sequences in or around the dabigatran-binding S4 subsite derived from naturally occurring serine proteases or plasma proteins were introduced in prothrombin.
A panel of prothrombin variants was generated and transfected into HEK293 cells to allow for stable protein expression. In some of the generated prothrombin variants comprising insertions in amino acid sequence 91-99 that is directly adjacent to the S4 subsite protein expression was severely impaired. This indicates that exchange of any surface-exposed serine protease or plasma protein region into the prothrombin protease domain is not necessarily compatible with protein expression. In contrast, exchange of the human prothrombin 91-99 sequence for that of human kallikrein 3 or targeted amino acid replacement of S4 subsite residue Ile174 resulted in prothrombin protein expression levels similar to wild-type prothrombin.
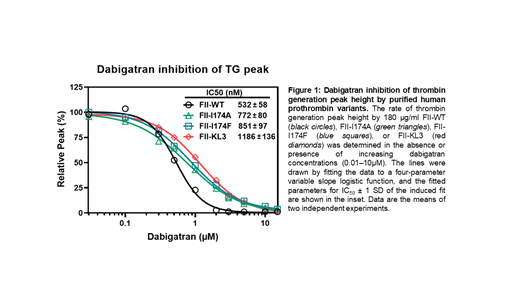
Following expression, prothrombin variants were purified to homogeneity using the CaptureSelect tm affinity matrix that selects for fully gamma-carboxylated prothrombin. The specific prothrombin clotting activity analyses of the purified prothrombin variants KL3 (0.7 ± 0.2 U/mg), I174A (0.8 ± 0.2 U/mg), and I174F (0.8 ± 0.3 U/mg) demonstrated an overall ~10-fold reduced specific activity relative to wild-type prothrombin (7.5 ± 0.1 U/mg). As such, modification of the S4 subsite likely interferes with the binding and subsequent conversion of fibrinogen by thrombin. To determine whether the prothrombin variants supported tissue factor-initiated thrombin formation in human plasma, prothrombin-deficient plasma was supplemented with increasing plasma concentrations of prothrombin variant (90-180 ug/mL). Consistent with their reduced specific clotting activity, 180 ug/mL prothrombin variant was required to obtain substantial thrombin generation but with reduced thrombin generation parameters (peak thrombin, ETP) relative to supplementation with plasma concentrations of wild-type prothrombin (90 ug/mL). This calibrated automated thrombin generation assay set-up was used to assess the DOAC-resistance of the prothrombin variants. While thrombin formation reached half-maximum inhibition at 532 ± 58 nM dabigatran in wild-type prothrombin-supplemented plasma, addition of the prothrombin variants displayed a ~2-fold reduced sensitivity to dabigatran inhibition (IC50: 1186 ± 136 nM prothrombin-KL3; 851 ± 97 nM prothrombin-I174F; 772 ± 80 nM prothrombin-I174A). This demonstrates that the S4 subsite-modified prothrombin variants are able to support thrombin generation in the presence of physiological plasma concentrations of inhibitor.
Collectively, our findings indicate that human prothrombin variants comprising a single point mutation at position Ile174 in the S4 subsite or at a region directly adjacent to the S4 subsite are able to generate thrombin in plasma inhibited by dabigatran. Hence, serine proteases with S4 subpocket modifications have the potential to bypass DOAC therapy and could provide a generic strategy in the development of novel DOAC-bypassing agents.
Reitsma: VarmX. B.V.: Current Employment, Current holder of individual stocks in a privately-held company, Current holder of stock options in a privately-held company, Patents & Royalties. Verhoef: VarmX. B.V.: Current Employment, Current holder of individual stocks in a privately-held company. Bos: VarmX B.V.: Research Funding; uniQure Biopharma B.V.: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal